📜Journal Club: Safe spontaneous breathing with helmet noninvasive ventilation in acute hypoxemic respiratory failure
By: Isabella Matos, Medica - 12/01/2025 19:13
👉🏼 In November 2025, the team led by the Italian researcher Massimo Antonelli from Gemelli Hospital in Rome, in partnership with the University of Toronto, composed of authors Tommaso Rosà🇮🇹, Luca S. Menga🇨🇦, Bruno L. Ferreyro🇨🇦, Domenico Luca Grieco🇮🇹, and Massimo Antonelli🇮🇹, published a review article in Current Opinion in Critical Care, highlighting the growing interest in helmet-based noninvasive ventilation (NIV) for managing hypoxemic patients due to its potential physiological and clinical benefits, summarized below:
Source: Rosà T, et al. Curr Opin Crit Care, 2025.
🫁 Key Principles
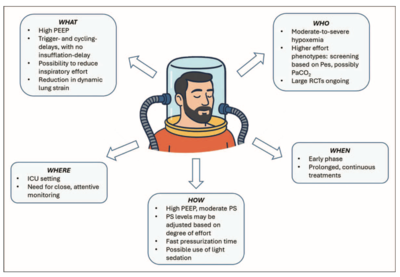
Helmet NIV may offer a valuable strategy for the noninvasive management of hypoxemic patients, particularly when applied early, for prolonged periods, and with settings aimed at minimizing injurious inflation in moderate to severe cases (PaO₂/FiO₂ < 200 mmHg). Compared with face masks, helmets facilitate the delivery of higher positive end-expiratory pressure (PEEP) during extended treatments, thereby improving oxygenation and mitigating harmful inflation patterns related to lung heterogeneity. This may help prevent patient self-inflicted lung injury (P-SILI).
🧩 Helmet NIV: WHAT
Helmets allow the application of higher PEEP levels, promoting lung recruitment, alveolar stabilization, reduced pulmonary heterogeneity, improved oxygenation, caudal diaphragmatic displacement, and decreased inspiratory effort. The interface’s inherently high compliance results in asynchrony that is not necessarily undesirable and may even be beneficial: delayed triggering and cycling, when ventilator valves are closed, allow patients to generate airflow or exhale into the helmet’s internal volume, preventing isometric contractions, the sensation of absent flow, and pendelluft phenomena.
Additionally, the decoupling between negative pleural pressure oscillations and the rise in airway pressure generated by the ventilator helps minimize respiratory increases in driving pressure, collectively contributing to reduced inspiratory effort and dynamic lung strain.
👤 Helmet NIV: WHO
Current guidelines do not provide conclusive recommendations for or against helmet NIV in hypoxemic patients.
Helmet NIV (with variable pressure support) appears more suitable for patients with high inspiratory effort, as high-flow nasal cannula (HFNC) and helmet continuous positive airway pressure (CPAP) are insufficient to manage this condition. Conversely, helmet CPAP and HFNC may be preferable for hypoxemic patients with mild inspiratory effort, offering oxygenation benefits without increasing lung stress. Overall, the most recent evidence suggests that helmet NIV may provide the greatest physiological and clinical benefits in patients with moderate to severe hypoxemia (PaO₂/FiO₂ < 200 mmHg), particularly those with significant inspiratory effort (>10 cmH₂O) or PaCO₂ < 35 mmHg.
⏳ Helmet NIV: WHEN
Early application of higher PEEP levels during the initial, more acute phase may yield the greatest benefit by reducing inspiratory effort, potentially decreasing lung stress and dynamic deformation, thereby attenuating the inflammatory cascade and slowing the progression of lung injury. Late initiation often coincides with lung injury progression toward more consolidated, less recruitable tissue, where PEEP’s benefits in reducing deformation are limited.
Prolonged and continuous helmet NIV sessions appear advisable to maximize efficacy until clinical improvement occurs.
🏥 Helmet NIV: WHERE
ICUs represent the ideal environment for helmet NIV due to the need for continuous specialized monitoring, immediate recognition of treatment failure, and rapid care escalation. Although its use in intermediate care or emergency settings is feasible, it requires adequate infrastructure and trained staff to ensure both patient safety and treatment effectiveness.
⚙️ Helmet NIV: HOW
Optimal interface performance requires high PEEP (10–14 cmH₂O), moderate-to-high pressure support (8–14 cmH₂O), and very short pressurization time. Pressure support should ideally be titrated to balance reductions in inspiratory effort with minimal increases in lung distending pressures. If substantial air leaks occur, helmet positioning must be adjusted.
A practical solution to minimize axillary skin breakdown is to pull the straps downward and anchor them to the patient's bed, keeping the helmet in place without increasing localized pressure. To reduce CO₂ rebreathing, a frequently cited concern, a dual-limb circuit should be used instead of a Y-piece, with ports positioned on opposite sides of the helmet. Light sedation may be employed, with dexmedetomidine preferred due to its minimal impact on neural respiratory drive, making it a safer option.
👉🏼 In this context, an article published by our group, MATOS, IM et al., in the Jornal Brasileiro de Pneumologia in 2024, entitled “CPAP delivered via a helmet interface in lightly sedated patients with moderate to severe ARDS: predictors of success outside the ICU”, used light sedation with dexmedetomidine in all patients treated with ELMO-CPAP outside the ICU setting. The study achieved a high success rate (avoidance of intubation) of 72.8%, with predictors of success including younger age, <75% lung involvement on HRCT, ROX index > 4.88 at the second hour of therapy, and prolonged duration of the first continuous ELMO-CPAP session (>24 hours). Older age and intubation were associated with mortality.
😉 Access the articles:
🧐 How do you choose the ideal interface for your patient with hypoxemic acute respiratory failure undergoing NIV?
🧐 How do these principles align with the new SBPT/AMIB Practical Guidelines for Mechanical Ventilation? We will comment on this in response to this post. Stay tuned!
To add an answer on this topic and read the replies...
You must have a valid and active xlung subscription
If you are already a subscriber, please Login at the top of the page, or subscribe now