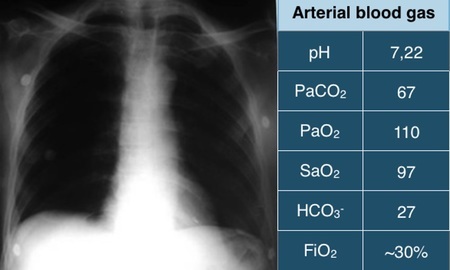
Patient with acute respiratory acidosis in oxygen therapy
Last update: Tuesday, 12 Nov 2019 at 16:23
A 52-year-old patient, non-smoker, comes to the emergency room with evident dyspnoea
one day after the onset of a common cold. Due to an 88% SpO2, on arrival, O2 was administered by a nasal catheter with a flow rate of 3 l / min.
Reported being diagnosed with Amyotrophic Lateral Sclerosis (ALS), 8 months ago.
He is alert and eager. The respiratory rate is 28 bpm, with the use of accessory musculature and paradoxical respiratory movement.
Lungs auscultation reveals reduced breath sounds in the lower fields.
Blood Pressure: 135x90 mmHg. Pulse: 106 ppm.
The chest X-ray and arterial blood gas, collected during oxygen therapy by nasal catheter at 3l/min, are shown below.
How would you manage his respiratory problems at the moment?
a) Remove the supply of O2 immediately
b) Indicate invasive mechanical ventilatory support
c) Indicate non-invasive ventilatory support (NIV)
d) Observe clinical response for the following hour
We invite you to comment on this exercise and suggest the correct answer or ask questions about it.
For this exercise we recommend reading the chapter Acute Respiratory Insufficiency in the MV Manual.
To continue reading...
You must have a valid and active xlung subscription
If you are already a subscriber, please Login at the top of the page, or subscribe now